NCDHHS Extends Open Enrollment for Medicaid Managed Care through May 21, 2021. Read about it in this announcement.
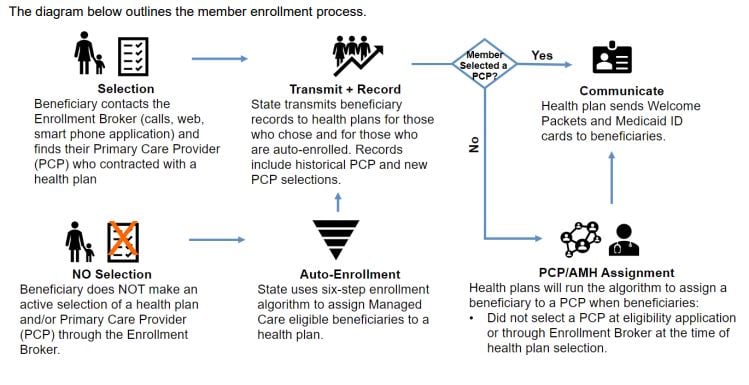
In NC Medicaid Managed Care, most beneficiaries choose their health plan and primary care provider (PCP) or Advanced Medical Home (AMH), which is a type of primary care provider. During open enrollment from March 15 through May 21, 2021, beneficiaries will enroll in a health plan and select their PCP/AMH. If a beneficiary does not select a health plan, they will be automatically enrolled in one by the NC Department of Health and Human Services (DHHS). If a beneficiary does not select a PCP/AMH, then the health plan will assign one to them. First, DHHS will auto-enroll the beneficiary in a health plan. Once the health plan receives the beneficiary information, the health plan will auto-assign a PCP/AMH to the beneficiary.
Auto-Enrollment in a health plan
If a beneficiary does not select a health plan, they will be automatically enrolled in one by the NC Department of Health and Human Services (DHHS) following the beneficiary open enrollment period. Beneficiaries will be able to change health plans up to 90 days after the effective date. For more information on auto enrollment in a health plan, please see the Medicaid Managed Care Member Enrollment: Part 1 – Health Plan Auto-Enrollment Fact Sheet.
Auto-Assignment to a PCP/AMH
If a beneficiary does not select a PCP/AMH, then the health plan will assign one to them. Beneficiaries will be able to change their PCP/AMH up to 30 days after they receive notice of their initial PCP/AMH assignment. For more information on health plan auto-assignment of PCP/AMHs, please see the Medicaid Managed Care Member Enrollment: Part 2 – PCP/AMH Auto-Assignment Fact Sheet.
Newly Eligible Medicaid Beneficiaries
After open enrollment ends, newly eligible Medicaid beneficiaries who are required to enroll in a health plan will be able to choose a plan and/or a PCP/AMH when they apply with a caseworker or through ePASS. If beneficiaries do not choose a health plan, DHHS will enroll them in a health plan. Health plan enrollments, whether selected by the beneficiary or through auto-enrollment, will be processed nightly. If the newly eligible beneficiary does not select a PCP/AMH, then the health plan will assign one to them within 24 hours.
Additional resources for providers on health plan auto enrollment and PCP/AMH auto assignment can be found on the Medicaid Managed Care Webinar Series for Providers under Beneficiary Attribution.
What if I have questions?
For general inquiries and complaints regarding health plans, NC Medicaid has created a Provider Ombudsman to represent the interests of the provider community. The Ombudsman will:
- Provide resources and assist providers with issues through resolution.
- Assist providers with Health Information Exchange (HIE) inquires related to NC HealthConnex connectivity compliance and the HIE Hardship Extension process.
Provider Ombudsman inquiries, concerns or complaints can be submitted to Medicaid.ProviderOmbudsman@dhhs.nc.gov, or received through the Provider Ombudsman line at 866-304-7062. The Provider Ombudsman contact information is also published in each health plan’s provider manual.
For questions related to your NCTracks provider information, please contact the General Dynamics Information Technology (GDIT) Call Center at 800-688-6696. To update your information, please log into NCTracks provider portal to verify your information and submit a Manage Change Request (MCR) or contact the GDIT Call Center.
For all other questions, please contact the NC Medicaid Contact Center at 888-245-0179.